Pressure ulcers are classified as chronic wounds, but the reason for poor healing is not well understood, and there is an unmed need for strategies to assess risk, prevent formation, and improve healing.
At the Tucker-Kellogg lab, we look at pressure ulcers as a research challenge of understanding tissue resiliency, injury response, oxidative stress, and regenerative self-assembly. We approach these challenges with computational methods and pre-clinical models.
Why are pressure ulcers worse than other wounds of the same size?
Why is there so much slough?
 One project is comparing fast-healing versus slow-healing wounds, looking at how they differ in the earliest stages, before any difference in healing arises. We find that poor-healing wounds have too much anti-microbial inflammation and not enough anti-debris inflammation, during the initial days after injury. In other words, immune cells are enacting programs like oxidative stress and extracellular traps that may be beneficial at fighting bacterial infection, but at the same time, immune cells in the wound bed are failing to provide sufficient phagocytosis -- they're neglecting to clear away debris and necrotic tissue. As expected, any failure of phagocytosis forces the body to expel the necrotic tissue through sloughing. In other words, dead tissue from fat layers, muscle layers, and dermal layers get pushed up and off the wound, while healthy cells proliferate below. Amazingly, this happens even if the experiment is conducted in a "cleanroom" with no bacteria or microbial pathogens at all! We found that a crucial determinant of whether immune cells carry out anti-microbial or anti-debris programs is the heme-carrying protein myoglobin. The same pathway can be targeted using iron chelation therapy.
One project is comparing fast-healing versus slow-healing wounds, looking at how they differ in the earliest stages, before any difference in healing arises. We find that poor-healing wounds have too much anti-microbial inflammation and not enough anti-debris inflammation, during the initial days after injury. In other words, immune cells are enacting programs like oxidative stress and extracellular traps that may be beneficial at fighting bacterial infection, but at the same time, immune cells in the wound bed are failing to provide sufficient phagocytosis -- they're neglecting to clear away debris and necrotic tissue. As expected, any failure of phagocytosis forces the body to expel the necrotic tissue through sloughing. In other words, dead tissue from fat layers, muscle layers, and dermal layers get pushed up and off the wound, while healthy cells proliferate below. Amazingly, this happens even if the experiment is conducted in a "cleanroom" with no bacteria or microbial pathogens at all! We found that a crucial determinant of whether immune cells carry out anti-microbial or anti-debris programs is the heme-carrying protein myoglobin. The same pathway can be targeted using iron chelation therapy.
Why should we pay attention to muscle, if this is a skin wound?
The Role of the Panniculus Layer in Prevention and Recurrence of Heel Pressure Ulcers
Multiple types of chronic wounds share a similar biochemical problem -- Iron

Many types of chronic wounds occur in blood vessels, where problem arise from the death of red blood cells and the release of hemoglobin proteins into the wound. (Patients see hemosiderin as a brown pigment around the wound.) Vascular ulcers are well-documented to have impaired regeneration because of this hemoglobin excess. The same mechanism has never before been linked to pressure ulcers. In our studies, very high levels of ferric iron were present in the wound bed of small deep pressure ulcers (centimeter wide, penetrating the panniculus muscle below the dermis). For comparison, muscle injuries without pressure showed no iron accumulation. In other words, the pressure injuries (which heal poorly) had too much iron, and the comparison injuries (which heal beautifully) had low iron. Knocking out myoglobin was sufficient to prevent build-up of iron in the wound bed and to improve all measures of abnormal damage. We conclude that muscle pressure ulcers have myoglobin-derived iron toxicity, similar to the hemoglobin-derived pathologies that are recognized in vascular ulcers.
Tissue damage can keep expanding after pressure is removed
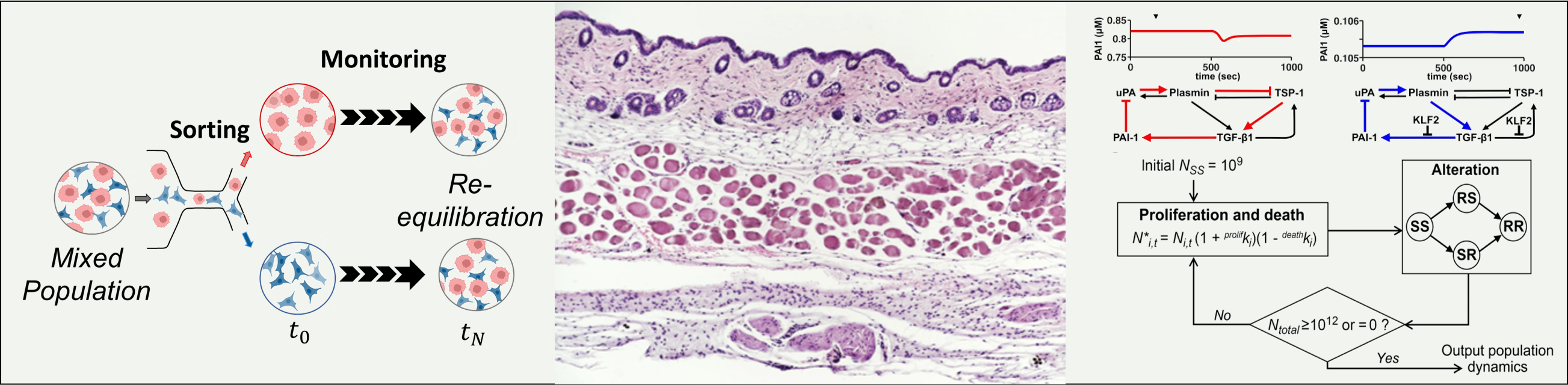
An initial injury can harm neighboring tissues, in a process called secondary progression of a wound. If cells die without first performing apoptosis, then they spill open to cause harm for neighboring cells. We found (J Biomechanics 49:1311) that when a stressful environment brings cells to a tipping point between survival and death, a tissue can be salvaged or killed by small influences such as myoglobin levels and oxidative stress, or by changing the cellular threshold between apoptosis and necrosis.


Three under-appreciated factors in pressure ulcer formation and propagation are membrane repair speed, oxidative feedback toward repair speed, and the contradictory effects of apoptosis versus necrosis, toward the spread of damage beyond an intial injury.
Although apoptosis can kill cells that would otherwise be viable, apoptosis also has the potential to limit permeabilization of cells that would otherwise rupture or lyse. In oher words, there is a range of injuries where apoptosis is actually helpful for salvaging tissue viability, provided it is well-tuned to occur before necrosis, and only in cells that would otherwise necrose. Therefore, therapies that target apoptosis might be most beneficial to tissue viability if they can be tailored to rectify the mismatch between apoptosis and necrosis, rather than simply fighting against death in every cell.